No Fee Accident Lawyers
Devastating Losses Call for Exceptional Litigators

Our team of New Hampshire and Massachusetts medical malpractice lawyers work hard to stay on top of the medicine. Medical malpractice, also known as medical negligence, occurs when the patient’s physician “deviates from the standard of care”. The legal definition of standard of care is as follows. “The degree of care or competence that one is expected to exercise in a particular circumstances or role”. A physician deviates from the standard of care when his actions fall below what is expected of the average physician. For the deviation to be actionable, it must be “causally related” to the patient’s injury. Favorable medical outcomes are not guaranteed. The mere fact that a patient has a poor result does not constitute medical malpractice. Chapter 507-E MEDICAL INJURY ACTIONS (state.nh.us)
Deviations from the standard of care can take many forms according to our New Hampshire and Massachusetts medical malpractice lawyers. Some examples include surgical error, failure to diagnose, and lack of informed consent. For every medical malpractice case that we review, we spend a considerable amount of time “learning the medicine”. This approach includes not just a review of the client’s medical records, but also the medical literature, guidelines, and textbooks. Additionally, this approach requires us to familiarize ourselves with all the different practice areas of medicine. This includes orthopedics, vascular surgery, oncology, general surgery, neurology, etc. If we are confident that the case has merit, and that medical negligence was committed, we go to great lengths to find the premier experts.
It is essential that the medical malpractice lawyer has specialized experience and the capital reserves to work the case up. The injuries are oftentimes catastrophic, the stakes are high, and the potential for a large recovery is always there. That is why the insurance company spares no expense in hiring the top attorneys and experts to defend the case. Your attorney must not only keep pace with his opponents, but he must proactively overwhelm them in a medical negligence case.
The lobby groups have been very aggressive in ensuring that there are laws on the books that protect doctors. New Hampshire required the plaintiff participate in a screening panel at the beginning of the case designed to deter lawsuits. MEDICAL MALPRACTICE SCREENING PANELS (RSA 519-B) | New Hampshire Judicial Branch (nh.gov). Fortunately, the plaintiff’s bar has been successful at fighting back. We were able to repeal the screening panel requirement effective July 2023. Welcome (nhaj.org)
Another positive aspect of bringing a medical malpractice case in New Hampshire, is that we have mandatory mediation. The medical malpractice lawyers hire a neutral party to oversee settlement negotiations before trial. The Granite Law Group takes pride in building the case up to negotiate considerable settlements for our clients. Mediation allows them to have control over the outcome of their case.
Below are several case studies that illustrate the types of medical malpractice matters we have worked on:
Our medical malpractice lawyers explain that the client underwent exploratory arthroscopic shoulder surgery. During the procedure, the surgeon performed a more intrusive technique called an open biceps tenodesis. This procedure involved making an open incision adjacent in the patient’s armpit. Then he used two metal retractors to expand the surgical field. He released the torn biceps tendon. Then he secured the tendon to the head of the humerus with an anchor.
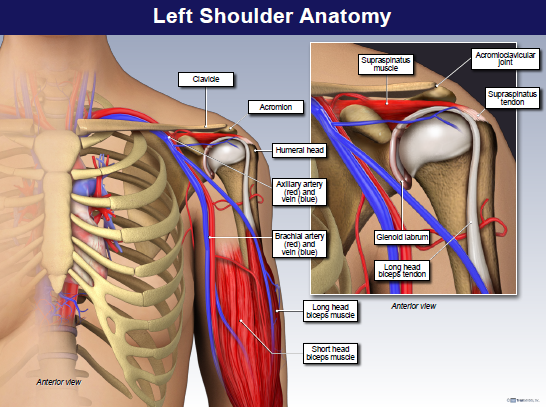
The surgeon placed one of his retractors too far medially causing it to lacerate the brachial artery. They discover the laceration when pressure from the retractor is released. The surgeon had already left the operating room to commence his next surgical case. This activity called performing “concurrent surgeries.”
A more egregious version of this practice is called “running two rooms”. This involves the surgeon performing two surgeries at the same time. The practice was uncovered at MGH by the Boston Globe. Clash in the name of care – A Boston Globe Spotlight Team Report
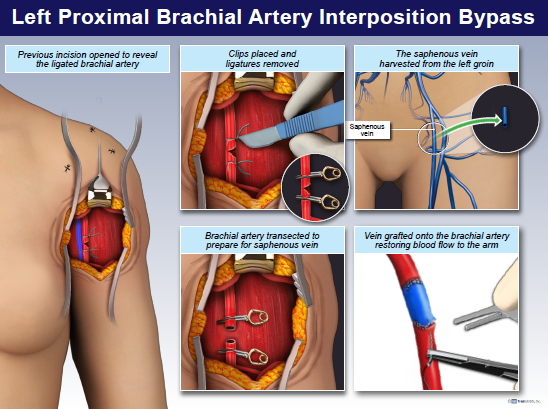
When the surgeon returned, he should have controlled the bleeding. Then he should have called the on-call vascular surgeon. Instead, he repaired the vessel himself with a ligation. Ostensibly, he tied off the vessel so he could start his next surgery. This was medical negligence.
No more than an hour later the patient lost her radial pulse. CTA imaging revealed a massive blood clot that completely occluded the artery. Acute Limb Ischemia: An Update on Diagnosis and Management – PMC (nih.gov)
They rush the patient to tertiary care. They identify the ligation. The silk ties are released, and perfusion is restored. The brachial plexus nerves are severely damaged. The patient sustained catastrophic damage to her arm.
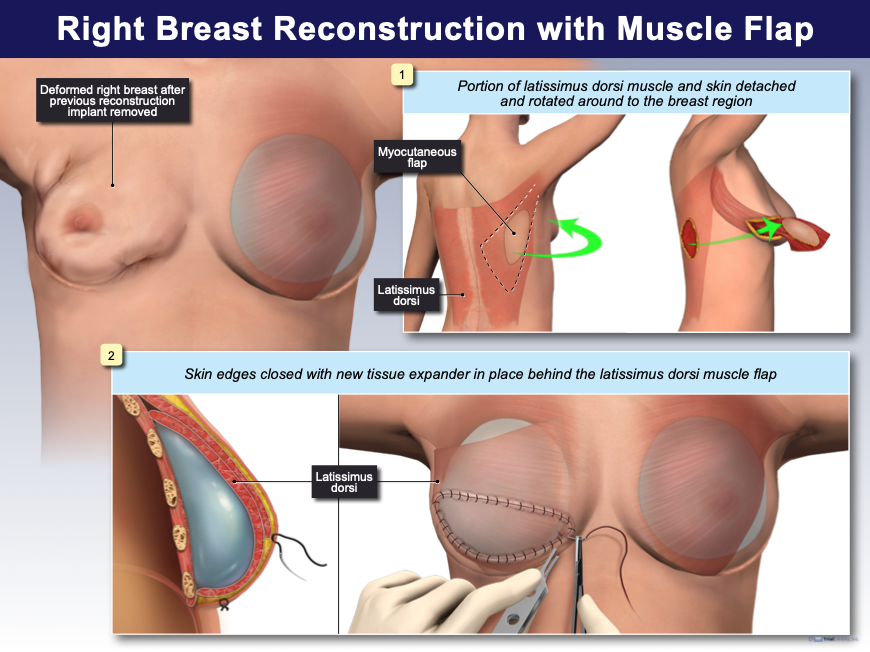
Our medical malpractice lawyers detail how the client had developed an abnormal breast lesion called atypical ductal hyperplasia (ADH). They remove the lesion. The patient feared she would develop a malignant growth with her family history. She chooses a radical bilateral prophylactic mastectomy. The surgeon pushes the procedure. During the breast reconstruction phase, the patient experienced horrific plastic surgery complications. After multiple failed surgeries, she had to undergo a dorsi latissimus flap procedure. This procedure transports muscle from the patient’s back to the chest wall to support the implant.
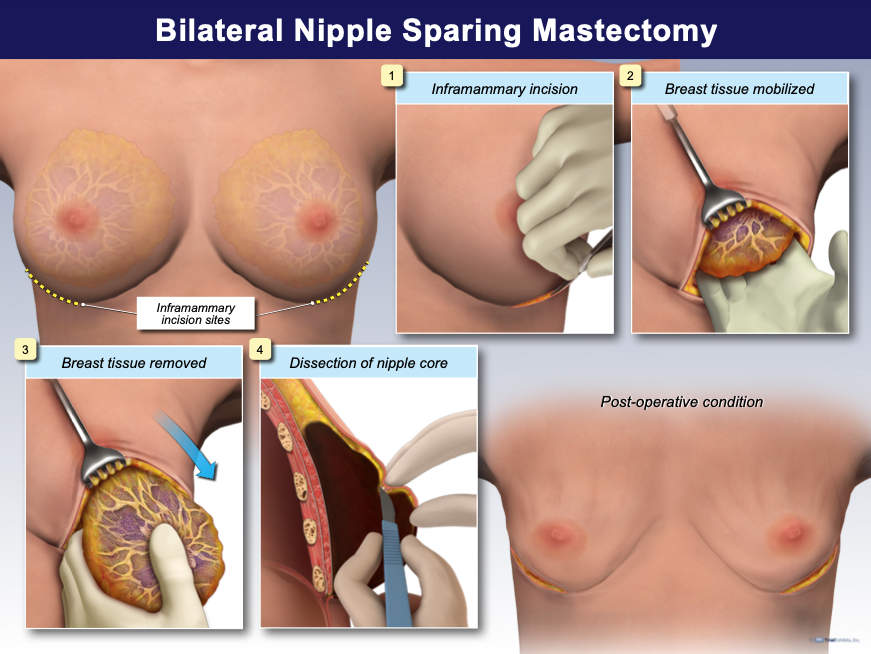
The issue was not a deviation in the plastic surgery phase of the case, but with the mastectomy itself. There was a lack of informed consent and the prophylactic procedure was wholly unnecessary. Breast cancer screening must use the Gail model. The model involves an algorithm where the patient’s risk calculation is provided as a percentage based on the past data collected. Breast Cancer Risk Assessment Calculator – NCI
In this case, the patient’s surgeon never administered the screening test before the mastectomy. The risk was much less than what she was led to believe by the surgeon. The patient’s mother subsequently underwent genetic testing for the BRCA1 and BRCA2 mutations. If positive, the patient’s risk of developing breast cancer would exponentially increase. ACS Breast Cancer Screening Guidelines | American Cancer Society. The patient was incorrectly led to believe that her family did in fact have the genetic mutation. It turned out that the testing came back negative.
This was medical negligence. The patient was never provided with the relevant information to make an informed decision about whether the mastectomy was necessary. Had she received that information, she never would’ve undergone the mastectomy and would’ve avoided all the resultant complications.
Our medical malpractice lawyers summarize the case. The patient has Mediport device placed to receive chemotherapy medication. The procedure involved inserting the device in the patient’s upper chest and threading a catheter through the superior vena cava. They can inject medication into the port. It then travels through the superior vena cava vein into the heart. It mixes with the deoxygenated blood. Blood is reoxygenated and distributed throughout the body via the arteries.
The standard of care in this case was to access the vessel utilizing the Seldinger technique. The technique involves inserting a guidewire through the vein under ultrasound guidance. A larger catheter sheath passes over the guidewire. The procedure carries the risk of perforating the vessel. Thus, if the surgeon encounters any resistance while threading the guidewire, he should back it out and try again. The surgeon can’t force it through.
In this case, the general surgeon forced the guidewire which perforated the vessel. The pericardium, a sack that encapsulates the heart, filled with blood. The patient died on the operating table. We proved the guidewire was forced. An x-ray study showed the guidewire perpendicular in the patient’s chest. Of course, this too was medical negligence.
Our team retained a general surgeon, emergency room surgeon, and an oncologist. We also created a custom medical animation which incorporated the evidence into the minute-by-minute chronology of events.